The Importance of Sedation for Certain Vet Procedures
Ensuring the Safety of Both the Animal and the Veterinarian
Pre-Procedure Assessment and Planning
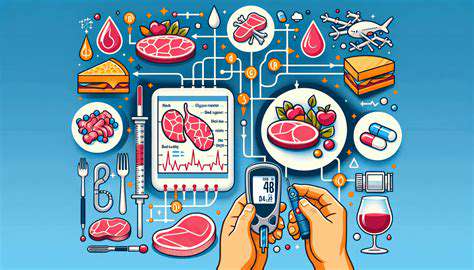
A crucial aspect of ensuring the safety of both the animal and the veterinarian during sedation procedures is a thorough pre-procedure assessment. This involves a detailed history of the animal's health, including any pre-existing conditions, allergies, or past anesthetic experiences. Veterinarians must also consider the animal's weight, breed, age, and overall physical condition to determine the appropriate anesthetic protocol. Careful consideration of these factors allows for a personalized approach that minimizes potential risks.
Proper Selection of Sedative Agents
Choosing the right sedative agent is paramount. Veterinarians must select agents based on the specific needs of the animal, considering factors like the duration of the procedure, the animal's temperament, and potential complications. This often involves consulting the latest research and guidelines to ensure the safest and most effective agent is used. The selection process should also involve a risk-benefit analysis to minimize any potential adverse effects.
Monitoring Vital Signs Throughout the Procedure
Continuous monitoring of vital signs, such as heart rate, respiratory rate, blood pressure, and oxygen saturation, is essential during the entire sedation procedure. This allows the veterinarian to quickly identify and address any adverse reactions or complications. Regular monitoring also helps in determining the appropriate adjustments to the sedation protocol, ensuring the animal's well-being throughout the procedure.
Proper Patient Positioning and Restraint
Appropriate positioning and restraint of the animal is critical to prevent injury to both the animal and the veterinarian. This involves using proper restraint techniques that minimize stress and discomfort for the animal, while ensuring the veterinarian has a clear line of sight and safe access to perform the procedure. Proper restraint is also essential for preventing the animal from injuring itself or the veterinarian.
Emergency Preparedness and Protocols
Having a comprehensive emergency plan in place is crucial for managing potential complications during sedation. This includes readily available emergency medications, equipment, and trained personnel to address any unforeseen events or adverse reactions. A well-defined emergency protocol ensures a swift and effective response to any critical situations that may arise during the procedure.
Post-Procedure Care and Recovery
Post-procedure care is just as important as pre-procedure assessment. This involves close monitoring of the animal's recovery, including vital signs and any signs of discomfort or complications. Providing appropriate supportive care, such as fluids and pain medication, is essential for a smooth recovery. The post-procedure period should be carefully managed to ensure the animal returns to its normal state as quickly and safely as possible.
Ethical Considerations and Communication
Ethical considerations must be paramount in every aspect of animal sedation. Open communication with the animal's owner about the risks and benefits of sedation is crucial. The veterinarian should explain the procedure, potential complications, and post-procedure care to ensure the owner's understanding and consent. This transparency fosters trust and ensures that the procedure is conducted responsibly and ethically.
Enhancing Diagnostic Accuracy and Treatment Effectiveness
Improving Diagnostic Efficiency
Diagnostic efficiency is paramount in modern healthcare. Faster and more accurate diagnoses translate directly to improved patient outcomes and reduced healthcare costs. Streamlining the diagnostic process, from initial patient interaction to final report generation, is crucial for achieving these goals. This involves optimizing workflows, leveraging advanced technologies, and fostering effective communication between healthcare professionals.
Implementing standardized protocols and utilizing electronic health records (EHRs) can significantly enhance the speed and accuracy of diagnostic procedures. These tools enable efficient data collection, storage, and retrieval, which allows clinicians to access relevant information quickly and make informed decisions. Furthermore, the use of sophisticated algorithms and artificial intelligence (AI) can assist in identifying patterns and anomalies that might be missed by human observation, leading to more precise diagnoses.
Optimizing Diagnostic Tools and Techniques
The continuous advancement of medical technology provides opportunities to refine existing diagnostic tools and develop new ones. Employing advanced imaging techniques, such as MRI and CT scans, allows for detailed visualization of internal structures, aiding in the identification of pathologies. Furthermore, the development of more sensitive laboratory tests and molecular diagnostics enables the detection of diseases at earlier stages, when intervention is most effective.
The integration of these advanced technologies into clinical practice can significantly improve diagnostic accuracy and facilitate timely interventions. This enhanced precision and speed will lead to better patient outcomes. Such advancements, when properly implemented, empower clinicians with more precise diagnostic tools, enabling swift and informed decision-making.
Enhancing Interprofessional Collaboration
Effective communication and collaboration among healthcare professionals are essential for improving diagnostic accuracy. This includes fostering strong relationships between physicians, nurses, radiologists, pathologists, and other specialists. Open communication channels enable the sharing of crucial information, insights, and potential diagnostic considerations, leading to a more comprehensive understanding of the patient's condition.
Collaborative efforts, facilitated by efficient communication systems and shared decision-making processes, can significantly improve patient care. By leveraging diverse perspectives and expertise, healthcare teams can arrive at more accurate diagnoses and develop more effective treatment plans. This collaborative approach is critical for optimizing patient outcomes.
Addressing Diagnostic Challenges in Diverse Patient Populations
Ensuring equitable access to high-quality diagnostic services for all patient populations is crucial. This necessitates addressing potential disparities in access to advanced diagnostic tools and expertise. In addition, consideration must be given to the unique needs of diverse patient groups, recognizing that cultural, socioeconomic, and linguistic factors can influence the diagnostic process.
Careful attention to these factors is paramount for achieving accurate and equitable healthcare outcomes. By adapting diagnostic approaches and protocols to the specific needs of diverse populations, healthcare providers can enhance the quality and accessibility of diagnostic services for everyone. This ensures that patients from all backgrounds receive the best possible care.
Choosing the Right Sedation Protocol for Specific Procedures
Choosing the Right Sedation Protocol for Your Patients
Selecting the appropriate sedation protocol is critical for ensuring patient safety and a positive experience during medical procedures. Properly chosen sedation protocols consider the patient's unique medical history, current health status, and the specific procedure being performed. This individualized approach minimizes risks and maximizes comfort, leading to better outcomes.
A thorough patient assessment is paramount. Factors like pre-existing conditions, allergies, and any history of adverse reactions to medications need careful consideration. This evaluation lays the groundwork for selecting a sedation protocol tailored to the patient's specific needs. Understanding the risks and benefits associated with different sedation techniques is crucial for informed decision-making.
Understanding the Different Types of Sedation
Various sedation options exist, each with its own level of consciousness-altering effects. Understanding the differences between conscious sedation, moderate sedation, and general anesthesia is essential for proper protocol selection. Different sedation levels correlate with varying degrees of responsiveness and the ability to maintain airway reflexes.
Conscious sedation, for example, allows the patient to maintain some level of responsiveness and cooperation. Moderate sedation, on the other hand, reduces anxiety and pain perception while still maintaining airway reflexes. General anesthesia renders the patient unconscious, completely eliminating pain perception and responsiveness.
The complexity of the procedure and the patient's overall health will determine the most appropriate level of sedation. Careful consideration of these factors is crucial for patient safety and comfort.
Developing a Comprehensive Sedation Plan
A comprehensive sedation plan involves more than just choosing a type of sedation. It also necessitates a detailed pre-procedure assessment, including a review of the patient's medical history, medications, and any potential allergies. This thorough preparation helps to identify potential risks and allows for proactive mitigation strategies.
Pre-procedure discussions with the patient are essential. This allows for clear communication regarding expectations, potential side effects, and the importance of following instructions. This communication fosters trust and reduces anxiety, ultimately contributing to a smoother and safer procedure.
Establishing clear communication channels between the medical team and the patient is vital. This includes outlining potential complications, monitoring procedures, and post-procedure recovery instructions. The goal is to ensure that everyone is on the same page and that the patient feels comfortable and informed.
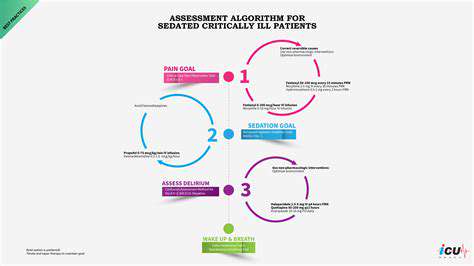
Monitoring and Managing Potential Complications
Post-procedure monitoring is critical for identifying and managing any potential complications. Continuous observation and vital sign checks are essential to ensure the patient's safety and well-being throughout the recovery period. A vigilant approach to monitoring allows for prompt interventions should any issues arise.
Having a well-defined plan for managing potential complications, such as respiratory depression or allergic reactions, is crucial. This plan should include clear protocols for administering medications, addressing potential complications, and contacting emergency services if necessary. A proactive approach minimizes risks and ensures a smooth recovery process.
Read more about The Importance of Sedation for Certain Vet Procedures
Hot Recommendations
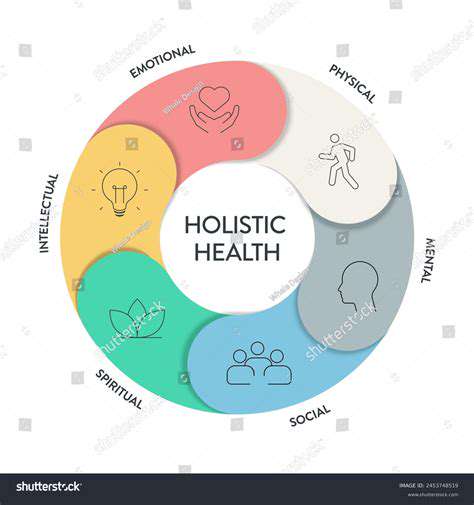
- Holistic Pet Health: Integrating Approaches
- The Future of Pet Identification: Biometric Scanners
- Service Dogs for PTSD: A Guide to Support
- The Benefits of Non Anesthetic Professional Teeth Cleaning
- Herbal Supplements for Pet Joint Health
- The Intersection of IoT and Pet Wellness
- Healthy Weight Management for Senior Pets
- The Best Pet Beds for Orthopedic Support and Comfort
- Competitive Dog Sports: Agility, Flyball, Dock Diving
- Luxury Pet Hotels: Pampering Your Beloved Pet