Leptospirosis in Pets: Understanding the Risk
What is Leptospirosis?
Understanding Leptospirosis
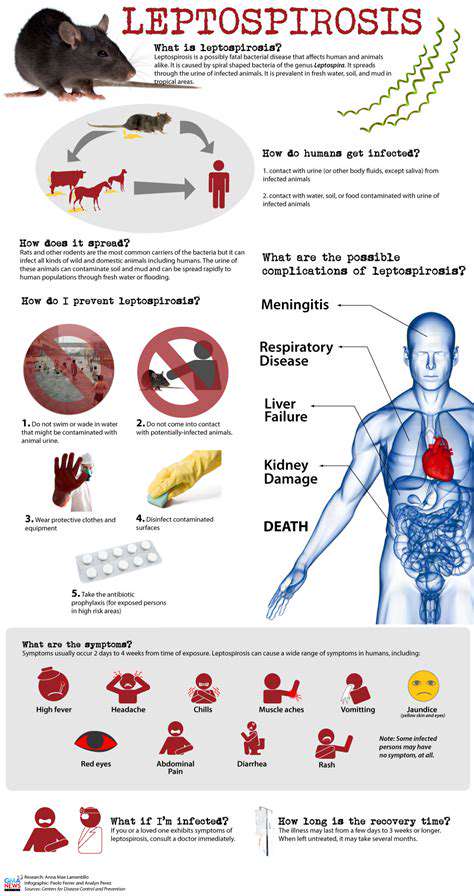
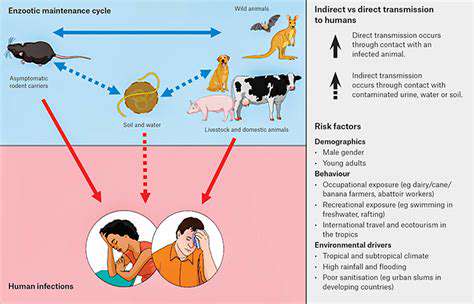
Leptospirosis represents a bacterial infection that spreads mainly via contact with contaminated water or soil. As a zoonotic disease, it can transfer between animals and humans. Transmission frequently happens when individuals come into contact with urine from infected animals, especially rodents, which pollute the surrounding environment. Grasping how this disease transmits proves vital for stopping its spread and preventing serious health consequences.
The Leptospira bacteria thrive in diverse animal hosts, making them widespread in nature. This prevalence underscores why protective steps and proper hygiene matter greatly in areas where exposure risks exist. Identifying these risk factors allows people to take precautions and reduce potential contact with the bacteria.
Symptoms and Their Variability
Leptospirosis symptoms vary widely from mild to severe. Early signs often resemble the flu, such as fever, headaches, muscle pain, and chills. Because these initial symptoms mirror other common illnesses, misdiagnosis can occur, delaying proper treatment.
In more critical cases, the infection may affect vital organs like the kidneys, liver, and lungs, causing dangerous complications. Detecting the disease early and initiating treatment promptly becomes essential to avoid these severe outcomes. Consulting a healthcare provider at the first sign of unusual symptoms could make a significant difference.
Diagnosing and Treating the Infection
Diagnosing leptospirosis combines clinical assessment with laboratory tests. Physicians review the patient's exposure history and symptoms, then conduct blood tests to confirm bacterial presence. Precise identification of the bacteria ensures the right treatment approach.
Treatment typically involves antibiotics, with the regimen adjusted based on infection severity. Starting treatment early minimizes complication risks and enhances recovery chances. Effective management relies on swift medical intervention.
Prevention Strategies
Preventing leptospirosis centers on avoiding contact with contaminated water and soil. Practicing good hygiene during activities like swimming or working in potentially infected areas is critical. Protective measures, such as wearing gloves or boots in high-risk environments, can further reduce exposure.
At-Risk Groups and Environmental Factors
Certain professions and populations face higher leptospirosis risks. Agricultural workers, veterinarians, and others in animal-related fields encounter environments with elevated rodent activity, increasing exposure likelihood. Environmental conditions, such as flooding, can amplify infection risks. Awareness and preventive actions help protect vulnerable groups.
People with preexisting health conditions may experience more severe complications if infected. Recognizing personal risk factors enables individuals to take appropriate precautions. Early medical attention remains crucial to prevent serious health issues.
Recognizing Leptospirosis in Pets
Early Warning Signs
Spotting early leptospirosis symptoms in pets is key to timely treatment. Detecting the disease early greatly improves recovery prospects. Initial signs often include lethargy and reduced appetite, which may seem minor but warrant attention. Owners should monitor their pets closely for behavioral changes.
Increased thirst or urination can also indicate infection. While subtle, these changes might signal underlying problems, especially alongside other symptoms. Consulting a veterinarian promptly ensures accurate diagnosis and care. Decreased energy levels and reluctance to engage in usual activities also serve as important clues.
Subtle physical changes, like altered posture or gait, may appear early. A slight limp or hesitation to move normally could hint at the disease. Behavioral shifts, such as avoiding playtime, should prompt a vet visit. These early signals, though mild, may necessitate swift action.
Severe Symptoms and Complications
Advanced leptospirosis can cause jaundice, evident through yellowing skin or eyes. This often coincides with vomiting, diarrhea, and appetite loss, leading to discomfort and weight decline. Addressing these symptoms quickly prevents worsening conditions.
Kidney problems may arise, marked by changes in urination patterns or blood in urine. Abdominal pain or tenderness suggests internal distress, requiring urgent veterinary care. Immediate attention is crucial to manage these serious complications.
Neurological issues, like seizures or tremors, indicate critical progression. These demand emergency intervention to stabilize the pet. Bleeding disorders, such as nosebleeds or gum bleeding, signal disseminated intravascular coagulation (DIC), a life-threatening condition. Rushing to the vet becomes imperative in such cases.
Read more about Leptospirosis in Pets: Understanding the Risk
Hot Recommendations
- Holistic Pet Health: Integrating Approaches
- The Future of Pet Identification: Biometric Scanners
- Service Dogs for PTSD: A Guide to Support
- The Benefits of Non Anesthetic Professional Teeth Cleaning
- Herbal Supplements for Pet Joint Health
- The Intersection of IoT and Pet Wellness
- Healthy Weight Management for Senior Pets
- The Best Pet Beds for Orthopedic Support and Comfort
- Competitive Dog Sports: Agility, Flyball, Dock Diving
- Luxury Pet Hotels: Pampering Your Beloved Pet