Cancer Treatment Options for Pets: From Chemotherapy to Immunotherapy
Understanding the Fundamentals of Chemotherapy
Chemotherapy remains a cornerstone in battling cancer, utilizing potent medications to attack rapidly dividing cells, a hallmark of malignant growth. These medications disrupt critical cellular functions, impairing the cancer cells' ability to multiply and survive. It's important to recognize that chemotherapy isn't universally identical; treatment plans are customized based on the patient's unique condition and cancer type.
Chemotherapy aims to reduce or eradicate tumors, enhancing the patient's quality of life and potentially prolonging survival. While effective, this approach may lead to various side effects, from manageable discomfort to more serious health concerns.
Targeting Specific Cancer Cell Pathways
Contemporary chemotherapy often focuses on disrupting specific pathways vital for cancer cell proliferation. By interfering with these mechanisms, treatment can slow or halt disease progression. Researchers continuously develop novel drugs designed to block these pathways more precisely, reducing harm to healthy tissues.
Identifying the genetic mutations and molecular drivers behind a particular cancer helps determine the most suitable chemotherapy protocol. This tailored strategy seeks to optimize treatment success while minimizing adverse effects.
Managing Chemotherapy Side Effects
While chemotherapy can be highly effective, it often causes side effects that vary by medication and individual response. Common issues include nausea, hair thinning, fatigue, and increased susceptibility to infections.
Effective management of these side effects is essential for maintaining patient comfort and treatment adherence. Supportive measures like anti-nausea drugs, pain relief protocols, and dietary adjustments significantly improve the treatment experience.
Diverse Chemotherapy Agents
The medical arsenal includes numerous chemotherapy drugs, each with distinct modes of action. Some disrupt DNA synthesis, while others inhibit cell division or trigger programmed cell death. Treatment selection considers multiple factors including cancer type, disease stage, and patient health status.
Major drug classes include alkylating agents, antimetabolites, cytotoxic antibiotics, and plant-derived compounds. Each category targets different aspects of cancer biology, allowing for customized treatment approaches.
Combination Therapy Strategies
Chemotherapy frequently complements other cancer treatments like surgery, radiation, and targeted therapies. This multimodal approach attacks cancer through multiple mechanisms, potentially improving outcomes.
Integrated treatment plans often yield superior results compared to single-modality approaches. By targeting various cancer cell vulnerabilities simultaneously, combination therapies may enhance effectiveness and survival rates.
Clinical trials continue to investigate optimal combinations, evaluating both efficacy and safety profiles.
Surgical Removal of Tumors: Precision and Potential for Cure
Preoperative Planning and Assessment
Tumor removal surgery demands thorough preoperative evaluation. This includes detailed imaging (CT, MRI, PET scans) to map the tumor's characteristics and relationship to adjacent structures. Comprehensive patient consultations outline procedural details, potential risks, and recovery expectations. These preparations enable surgeons to optimize their approach and reduce complications.
Pre-surgical testing assesses patient fitness and identifies any conditions that might affect outcomes. This holistic evaluation supports personalized treatment planning tailored to individual patient needs.
Surgical Techniques and Approaches
Surgical methods vary based on tumor location, size, and patient anatomy. Minimally invasive techniques (laparoscopic/robotic surgery) offer advantages like smaller incisions, less pain, and quicker recovery. Conventional open surgery may be necessary for complex cases.
Surgeon expertise guides technique selection, with advanced instrumentation enhancing precision. Meticulous tissue preservation during tumor removal helps maintain vital functions.
Post-Operative Care and Recovery
Recovery involves close monitoring, pain control, and appropriate medication. Rehabilitation programs aid in restoring function. Recovery duration depends on surgical complexity and individual health factors.
Patients must adhere to post-operative instructions regarding diet, activity, and medications. Regular follow-up appointments monitor healing and address concerns, promoting optimal recovery.
Potential Complications and Outcomes
While potentially curative, surgery carries risks including bleeding, infection, or tissue damage. These risks depend on tumor characteristics and patient health. Surgical teams implement rigorous precautions, though complications remain possible.
Immunotherapy: Harnessing the Body's Defense System
Harnessing the Immune System to Fight Cancer
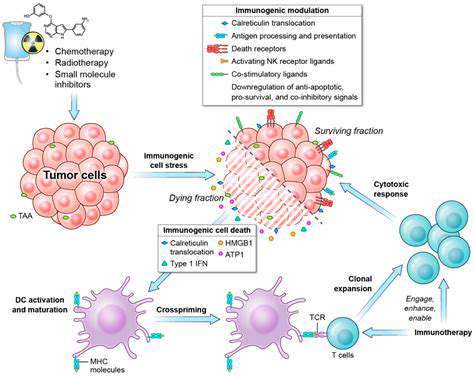
Immunotherapy marks a paradigm shift in cancer care, utilizing the body's natural defenses to combat malignancies. Unlike conventional treatments that indiscriminately damage cells, immunotherapy specifically enhances immune recognition of cancer cells.
This approach offers targeted action with potentially fewer side effects, particularly valuable for advanced or recurrent cancers where traditional therapies show limited effectiveness.
Key Mechanisms of Immunotherapy
Checkpoint inhibitors represent a major breakthrough, removing molecular brakes that constrain immune activity. Other approaches involve modifying immune cells (like T cells) to better recognize and destroy tumors.
Types of Immunotherapy Treatments
Current options include checkpoint inhibitors (e.g., pembrolizumab) and adoptive cell therapies, where modified immune cells are reintroduced to attack cancer. Each method presents unique benefits and implementation challenges.
Potential Benefits and Challenges
While offering improved outcomes and reduced toxicity for some patients, immunotherapy can cause immune-related adverse events. Cost barriers and variable response rates remain significant considerations in treatment planning.
Future Directions and Research
Ongoing studies explore combination therapies and novel immune-modulating approaches. Understanding tumor-immune interactions promises more effective future treatments, making immunotherapy a rapidly evolving field.
Read more about Cancer Treatment Options for Pets: From Chemotherapy to Immunotherapy
Hot Recommendations
- Holistic Pet Health: Integrating Approaches
- The Future of Pet Identification: Biometric Scanners
- Service Dogs for PTSD: A Guide to Support
- The Benefits of Non Anesthetic Professional Teeth Cleaning
- Herbal Supplements for Pet Joint Health
- The Intersection of IoT and Pet Wellness
- Healthy Weight Management for Senior Pets
- The Best Pet Beds for Orthopedic Support and Comfort
- Competitive Dog Sports: Agility, Flyball, Dock Diving
- Luxury Pet Hotels: Pampering Your Beloved Pet